Undergoing orthognathic surgery, more commonly referred to as jaw surgery, is a significant undertaking that requires careful planning, not only for the procedure itself but for the inevitable and often intense period of post-operative recovery. The pain experienced following this type of maxillofacial intervention is a complex, multifaceted sensation rooted in bone manipulation, soft tissue inflammation, and nerve response. It is a pain that cannot be dismissed as a simple ache; it often manifests as a deep, throbbing pressure that peaks shortly after the procedure before gradually subsiding. Effective management is therefore not a passive process of waiting for relief, but an active, structured strategy employing a range of pharmacological, physical, and nutritional tactics. This structured approach is fundamental to ensuring patient comfort, promoting healing, and facilitating a quicker return to routine, moving the patient through the initial acute phase of discomfort toward a sustainable recovery trajectory that avoids common pitfalls.
…it initiates a profound, multi-system biological cascade that alters the mechanical, electrical, and chemical environment of the heart and the entire vascular network.
The foundation of modern post-operative pain control, particularly after extensive procedures like jaw surgery, rests on the principle of multimodal analgesia. This strategy involves the simultaneous use of different classes of pain relievers, each targeting a distinct mechanism in the pain pathway. By combining non-opioid medications, primarily Non-Steroidal Anti-Inflammatory Drugs () like ibuprofen, with acetaminophen (paracetamol), clinicians can achieve superior pain relief with a reduced reliance on narcotic (opioid) painkillers. For example, ibuprofen, typically prescribed in doses such as 600mg every six hours, acts by reducing inflammation, which is a major source of post-surgical pain. Acetaminophen complements this by elevating the pain threshold. This combined, rotating schedule allows for consistent pain coverage, preempting the return of severe discomfort rather than reacting to it once it has fully established itself.
…By combining non-opioid medications, primarily Non-Steroidal Anti-Inflammatory Drugs () like ibuprofen, with acetaminophen (paracetamol), clinicians can achieve superior pain relief with a reduced reliance on narcotic (opioid) painkillers.
The utility of prescribed opioid medication is a topic that demands an intentional and conservative approach in the context of jaw surgery recovery. While a prescription for stronger pain relief may be provided, often to manage the sharpest initial discomfort that arises in the first three to four days, its use should be judiciously managed and swiftly tapered. Opioids are typically reserved for breakthrough pain that is not adequately controlled by the non-opioid regimen. They carry the risk of undesirable side effects, notably constipation and nausea, both of which can significantly complicate an already challenging recovery. When utilized, it is essential to take them with a small amount of food to mitigate gastric upset, and patients should be encouraged to transition back to the combined /acetaminophen regimen as soon as the acute post-surgical period subsides, recognizing that prolonged use is neither necessary nor advisable for the vast majority of patients.
…its use should be judiciously managed and swiftly tapered…
Beyond pharmacological intervention, the diligent application of physical therapies constitutes an indispensable pillar of effective pain and swelling management. Swelling, or edema, is an expected and entirely normal biological reaction to the bone and tissue trauma involved in jaw surgery, generally peaking around 48 to 72 hours post-operation. Immediate, continuous application of cold therapy is crucial during this phase. Ice packs, gel packs, or even bags of frozen peas wrapped in a light cloth should be applied to the exterior of the face over the surgical sites in intervals, such as twenty minutes on and twenty minutes off, for the first one to two days. This intense vasoconstriction helps to minimize the initial inflammatory response. After the 48-hour mark, when cold therapy loses its primary effectiveness, a transition to gentle moist heat can be beneficial to aid in muscle relaxation, alleviate stiffness, and encourage the reabsorption of residual bruising.
…Immediate, continuous application of cold therapy is crucial during this phase.
The post-operative diet presents a critical, often underestimated, factor in pain control and overall healing. The sheer act of chewing, yawning, or even excessive talking can exacerbate pain by stressing the healing bone and soft tissues. Strict adherence to a prescribed non-chew or liquid diet is mandatory for the initial recovery phase, typically the first one to two weeks, depending on the specific surgical plan. The composition of this liquid diet must not be neglected; while comfort foods like ice cream and broth are easily tolerated, the body requires adequate calories, protein, and essential nutrients to fuel the intensive healing process. Nutritional supplements, high-protein shakes, and carefully pureed meals (such as meats blended with gravy or creamy soups) are necessary to ensure that the patient’s nutritional demands are met without compromising the surgical fixation and exacerbating localized discomfort.
…The sheer act of chewing, yawning, or even excessive talking can exacerbate pain by stressing the healing bone and soft tissues.
The positioning of the body, particularly during sleep and rest, plays a subtle yet significant role in managing facial swelling and the associated pressure-based discomfort. The simple act of maintaining head elevation above the level of the heart, especially for the first few nights following the procedure, utilizes gravity to aid in fluid drainage from the surgical site. Sleeping with the head elevated on two or three pillows, or using a recliner chair, is strongly advised. This practice not only assists in minimizing edema but also contributes to better airway management, which can be temporarily compromised due to internal swelling and nasal congestion, particularly after upper jaw surgery. A comfortable, elevated resting position is an easy, non-pharmacological means of pain mitigation.
…The simple act of maintaining head elevation above the level of the heart, especially for the first few nights following the procedure, utilizes gravity to aid in fluid drainage from the surgical site.
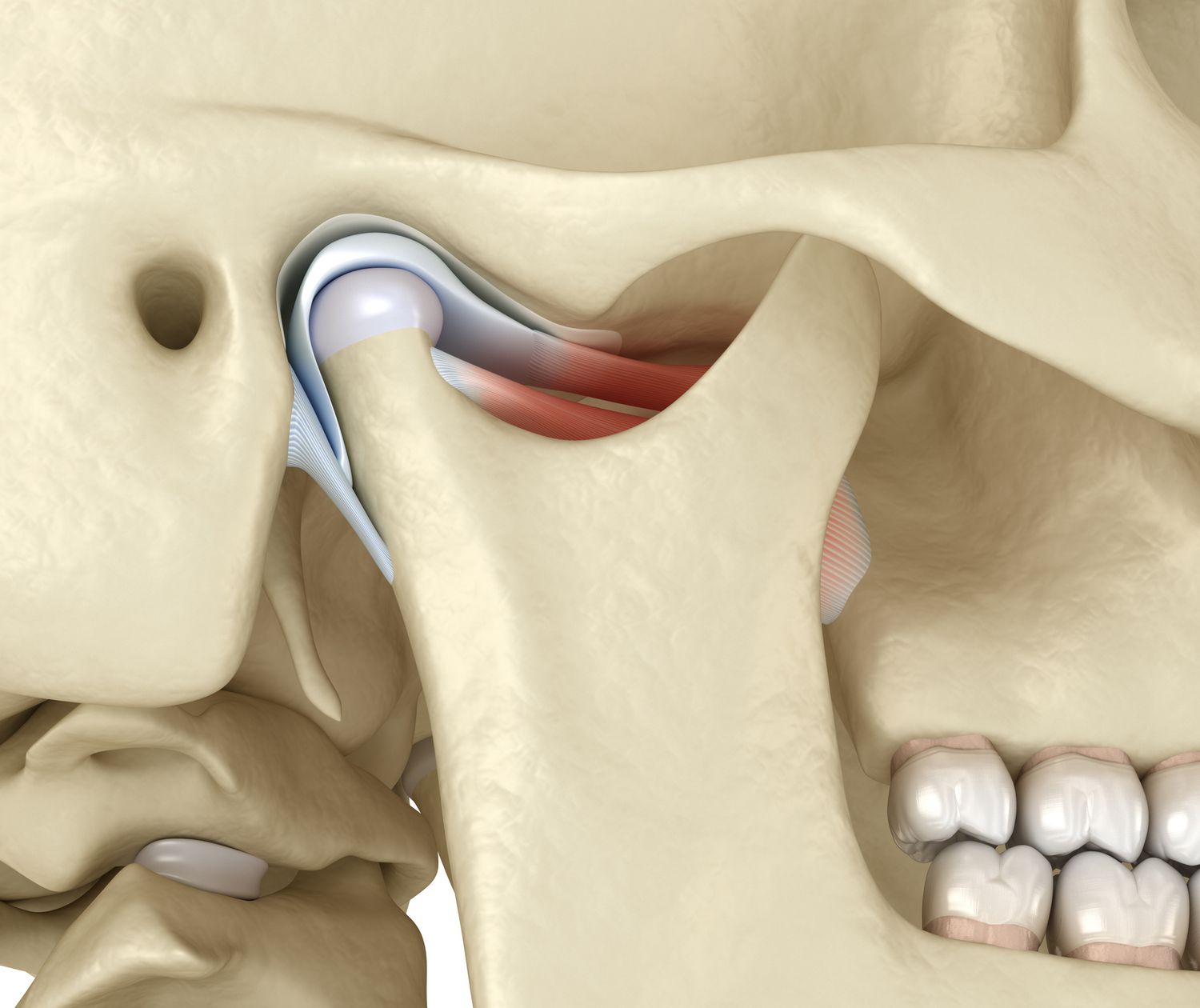
Post-surgical discomfort is also intimately linked to the temporary restrictions in jaw movement. Stiffness, or trismus, is a common sequela of the surgery, often making even small jaw movements or essential hygiene practices difficult. While aggressive movement is contraindicated, avoiding all movement leads to muscle and joint stiffness, which itself becomes a source of pain. After the initial period of immobilization (which may involve temporary intermaxillary fixation), and only upon the surgeon’s explicit instruction, gentle, controlled exercises are introduced. These slow, progressive stretches and mobilization routines are designed to restore the full range of motion. Early, cautious re-engagement with these exercises prevents long-term stiffness and reduces the muscular discomfort associated with disuse.
…While aggressive movement is contraindicated, avoiding all movement leads to muscle and joint stiffness, which itself becomes a source of pain.
Patients who have undergone upper jaw surgery (Le Fort I osteotomy) must be uniquely vigilant regarding nasal and sinus precautions, as neglecting these can indirectly increase facial pressure and discomfort. Swelling inside the nasal passages is expected and can lead to a feeling of intense pressure that can be mistaken for or exacerbate bone pain. Patients are strictly instructed not to blow their nose for a significant period—often six weeks—to prevent air from being forced into the soft tissues, which causes additional, painful swelling. Over-the-counter decongestant nasal sprays, when approved by the surgeon, can be used to help alleviate congestion, indirectly managing the associated facial pressure and contributing to a more comfortable recovery.
…Patients are strictly instructed not to blow their nose for a significant period—often six weeks—to prevent air from being forced into the soft tissues, which causes additional, painful swelling.
Oral hygiene post-jaw surgery is a non-negotiable component of recovery that is intrinsically linked to infection prevention and pain avoidance. While the mouth will be tender, incisions must be kept clean to prevent bacterial accumulation that could lead to an abscess or systemic infection, both of which would dramatically intensify pain. Gentle rinsing with a warm saltwater solution (a half-teaspoon of salt in a glass of warm water) should be performed after every meal. Tooth brushing is permitted, but often requires a small, soft-bristled, child-sized toothbrush to navigate the restricted opening and tender areas near the surgical sites. This meticulous, albeit difficult, routine is essential to prevent complications that would inevitably result in a significant spike in discomfort and a prolonged healing time.
…This meticulous, albeit difficult, routine is essential to prevent complications that would inevitably result in a significant spike in discomfort and a prolonged healing time.
A careful understanding of the expected pain curve and the warning signs of complications is necessary for patient self-monitoring and comfort. While pain is expected to be most bothersome in the first three days and gradually improve thereafter, any sudden, unexpected increase in pain after the first week, or persistent, severe pain that does not respond to prescribed medication, warrants immediate communication with the surgical team. Similarly, an increasing, localized swelling or the development of a fever greater than (
) could be indicative of an infection or other issue requiring prompt evaluation. The patient’s pain experience is a vital communication tool, and vigilance regarding these anomalies is a critical part of the post-operative management strategy.
…a careful understanding of the expected pain curve and the warning signs of complications is necessary for patient self-monitoring and comfort.
The psychological dimension of post-surgical recovery, often characterized by anxiety, sleep disruption, and frustration over dietary restrictions, should not be discounted in the overall pain experience. Managing pain effectively contributes significantly to improving sleep quality, which is vital for the body’s repair mechanisms. Patients should focus on maintaining realistic expectations, accepting that discomfort is a temporary phase of the healing process, and utilizing support networks. Distraction techniques, gentle activity within prescribed limits (short walks around the house), and addressing underlying anxiety can lower the subjective perception of pain, making the entire recovery period more tolerable and allowing the patient to focus their energy on adherence to the physical and nutritional protocols.
…The psychological dimension of post-surgical recovery, often characterized by anxiety, sleep disruption, and frustration over dietary restrictions, should not be discounted…
Structured pain management after jaw surgery is the disciplined application of combined pharmacological and physical strategies to harness the body’s healing capacity.
